To confirm the safety and performance throughout the expected lifetime of your medical device or IVD, this includes:
The data generated through the selected PMCF activities will inform your Post Market Surveillance (PMS) and your Clinical Evaluation Report (CER)/Performance Evaluation report (PER).
Your Post Market Clinical Follow-up Plan should include both general and specfic activities with a clear goal for these activities. What data are you looking to generate? Are the methods appropriate?
To answer these questions, you need to consider the varied options of PMCF activity.
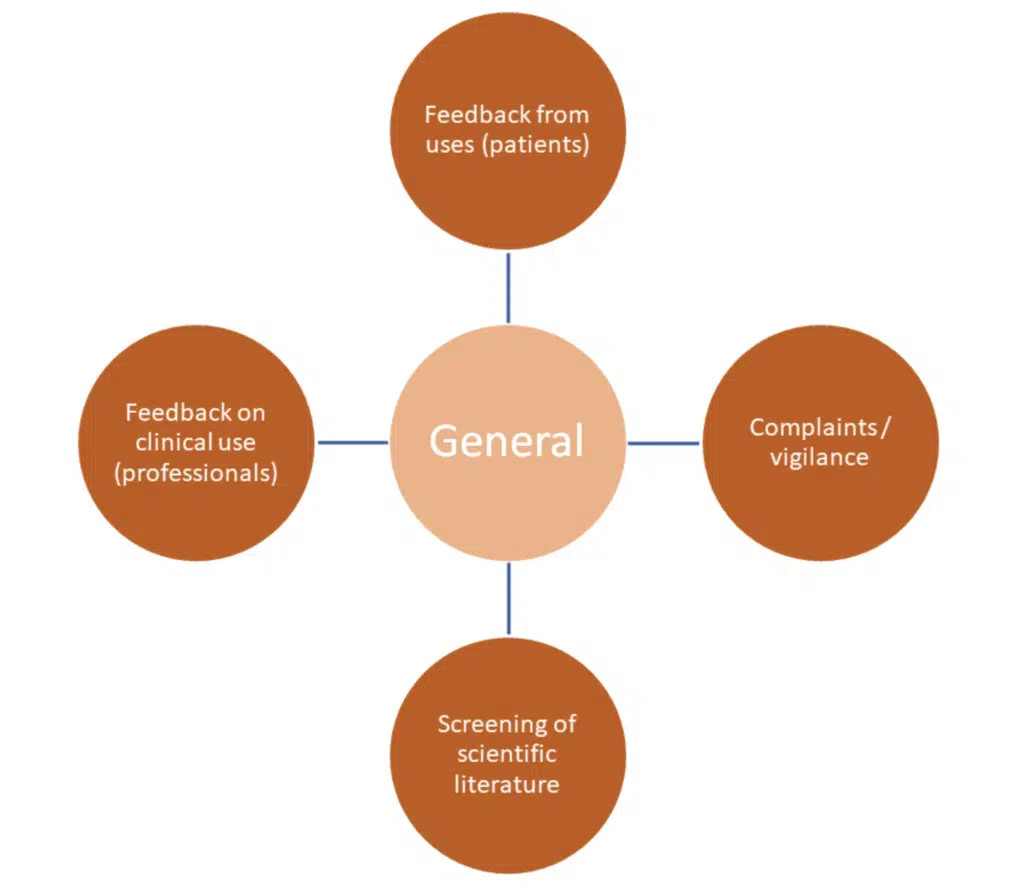
General activities are INFORMATION GATHERING in nature – often general subjective data, which by themselves do not provide a manufacturer with robust scientific evidence to demonstrate safety and performance. They should be used in conjunction with specific activities.
These methods are often subject to bias and variability across sources.
Some of the key challenges:
Literature review – limited data on the product under review, poor quality of the literature. There is also considerations to be had around the use of equivalent devices and the literature published on that devices. If equivalence is to be used, there must be a clear demonstration of equivalence – please review MDCG 2020-5 and get in touch if in doubt.
Access to patients and users: do you have adequate access, consent and data protection in place?
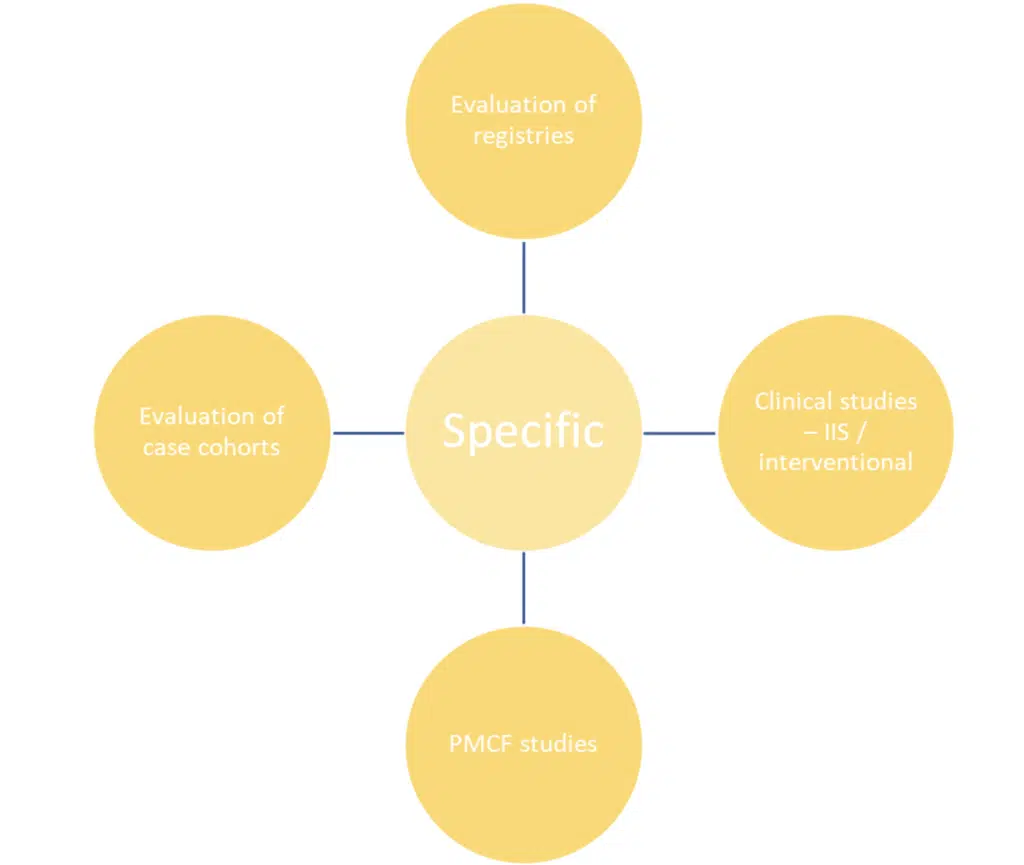
Specific methods are exactly that – more specific and more tailored to generating a scientifically significant dataset. They have a more defined purpose, population and defined dataset – if well done, these activities will provide you with the raw data on your product to support the demonstration of safety and performance.
Whatever activities are chosen, the PMCF Plan must have a clear justification for the choice.
Note: they are considered mandatory for products that:
These studies should have defined protocols – setting out as a minimum: defined population & sample size, inclusion and exclusion criteria, appropriate objectives & endpoints and follow-up.
There may be a need for ethical and competent authority approvals.
A PMCF study, as with a pre-clinical study, should be in-line with the expectations of ISO 14155:2020
Challenges:
Registries: This could be a product specific registry or a bigger product type registry – again either across a smaller population or area or indeed national such as the National Joint Registry.
A well designed and well used registry can be a great source of raw data for your product. A full analysis has the protetnial to product scientifical valid data around safety and performance.
Challenges:
To set and operate can be costly.
Limited reach – gaining patient and healthcare professional input can be challenging as often not possible to mandate.
Larger more national/global registries may only hold limited relevant data for the purpose of PMCF. Considerations should always be given to the utility of the data.
Surveys offer a degree of flexibility, they can be general but also designed to be highly specific – they can meet a wide range of needs in data generation.
General surveys tend to be retrospective design – asking the end-user to recall information on the device and its use.
Specific surveys can be patient level and case specific – this can be a single survey or a series of surveys that follow the usage of the devices (prospective). This could be direct to the patient or via a healthcare professional using patient records. The data obtained from this type of activity will be of higher quality – usually producing clinical data on the devices under review via patient outcome data and clinical indication data.
They also are considered relatively easy to design and conduct.
However, they should be used appropriately and as with all the activities their use needs to be justified within the PMCF plan.
Challenges:
Challenges:
Annex XIV Part B
6.2. The PMCF plan shall include at least:
This is what is required as a MINIMUM. PMCF plans should be designed to product real world evidence on your device’s safety and performance under normal use. This is longitudinal data collection, providing evidence on the safety and performance for the lifetime of the product.
The plan needs to be detailed with clear justification for the activities chosen – how will they generate the data you are seeking to evaluate. What is relevant for your device!?
Use the PMCF plan template provided in MDCG 2020-7!
MDCG 2020-8 provides guidance and a template for the report.
A PMCF report should:
Critical to remember that this report is taken in to consideration when updating the CER for your product. There are a number of considerations when reviewing the conclusions of the PMCF cycle.
This is a technical document and it should be clearly presented, and a scientifically robust conclusion with a focus on safety and performance of the product. It is a living document that needs to be updated and considered carefully.
If there are gaps – this often happens. If you discover ‘data gaps’ or a lack of demonstration in a particular area, then this needs to be reviews and evaluated. It should be demonstrated and be part of the conclusions. If it is a significant gap, then further activities may need to be considered and agreed on with you Notified Body (if relevant). Smaller gaps, maybe justified, but mitigations should be put in place to address them moving forward. Each circumstance is different, and the decision will need clear justification and be documented.
There is a significant increase in scrutiny by the NB under the new regulations. There are key timepoints at which the NB is likely to review your PMCF plan and data:
This is not an exhaustive list – just the key points of review – again it is a demonstration of that ‘lifecycle’ approach and that consistent review across that lifecycle.
It is not just a box to tick – it is a critical function that will build the knowledge of your device, allowing for that reassurance that your product continues to perform and that the benefit risk ratio continues to be acceptable and risks are mitigated as far as possible.
Relevent guidance:
MDCG 2020-7 PMCF plan template: A guide for manufacturers and notified bodies
MDCG 2020-8 PMCF Evaluation Report: A guide for manufacturers and notified bodies
MDCG 2021-6 Q&A on clinical investigations
MEDDEV 2.12/2 – Post Market clinical follow up studies
Subscribe to our newsletter
VISIT US
ECLEVAR FRANCE:
231 rue Saint-Honoré, 75001 Paris, France
ECLEVAR GMBH
ERFURT, Erfurt Hauptbahnhof
4th, 5th floor
Bahnhofstr. 38 Erfurt 99084
ECLEVAR Australia
Umina Beach NSW 2257, Australia
ECLEVAR UK Limited
3rd Floor 207 Regent Street, London, W1B 3HH
CONTACT US